The most common cause of Prostatitis is a bacterial infection in the prostate. Bacteria can get into the prostate when infected urine flows backwards from the urethra, which is not contagious through sexual contact. This is the leading cause of the chronic pelvic pain syndrome (CPPS), which occurs in approximately 1 out of 3 people assigned male at birth (AMAB).
Bladder infections, bladder stones, sexually transmitted infections (STIs), using a urinary catheter, prostate biopsy, prostate stones, urinary retention or urinary blockage, UTIs, and injury to the pelvic area are also the causes of prostatitis.
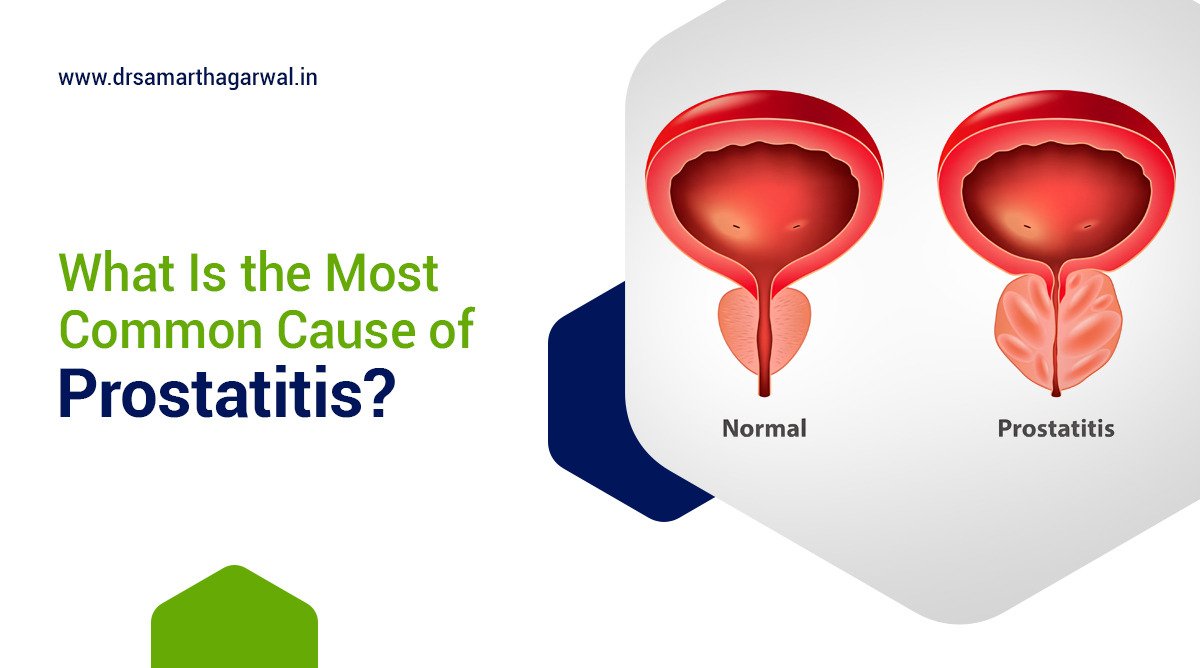
What is prostatitis?
Prostatitis is a disorder associated with inflammation of the prostate gland, found in men. This condition usually causes painful or difficult urination and pain in the groin, pelvic area, or genitals. While bacterial infections cause some, but not all, cases of prostatitis, there are four types, namely:
- Acute Bacterial Prostatitis (ABP): ABP causes the prostate to swell due to a bacterial infection and occurs in a bimodal distribution, mostly affecting young men (under 35 years) and elderly men (over 50 years).
- Chronic Bacterial Prostatitis (CBP): CBP develops gradually, causing irritative and obstructive symptoms but generally without the acute bacterial infection-related signs found in ABP.
- Chronic Prostatitis or Chronic Pelvic Pain Syndrome (CPPS): CPPS usually occurs in men younger than 50 and has no definite underlying bacterial cause. Symptoms such as pain in the lower abdomen, groin, penis, scrotum, or upper thighs, along with burning and frequent urination, persist or worsen.
- Asymptomatic Inflammatory Prostatitis: Men affected with asymptomatic inflammatory prostatitis do not show any symptoms or prostate-related issues; its presence is discovered only when medical tests are conducted for other urological or reproductive concerns.
Bacterial infections in the prostate may spread from other parts of the urinary or reproductive systems. Risk factors for prostatitis include previous prostatitis, infection of the urinary or reproductive system, HIV infection or AIDS, and the use of a urinary catheter or having a prostate biopsy.
Complications of acute or chronic prostatitis can include bacterial infection of the blood (bacteremia), inflammation of the coiled tube attached to the back of the testicle (epididymitis), pus-filled cavity in the prostate (prostatic abscess), infection that spreads to the upper pelvic bone or lower spine, and complications of chronic prostatitis/chronic pelvic pain syndrome, such as sexual dysfunction.
Diagnosis: Prostatitis may be diagnosed through a combination of methods, including digital rectal exam, urinalysis, prostate-specific antigen (PSA) testing, and transrectal ultrasound. Treatment for bacterial prostatitis involves antibiotics, while nonbacterial prostatitis may require other therapies, such as alpha-blockers, nonsteroidal anti-inflammatory drugs (NSAIDs), and physical therapy for pelvic floor muscle dysfunction. Acute bacterial prostatitis is a medical emergency, and prompt treatment is crucial. Prevention measures include practicing safe sex to prevent prostatitis caused by sexually transmitted infections and maintaining good urinary hygiene.
Treatments: Treatment approaches include behavioral modifications (such as maintaining hydration, avoiding specific foods, taking OTC pain relievers, warm baths, and Pelvic floor physical therapy), Antibiotics, Muscle Relaxants, Anti-inflammatory pain medication, and Prostate rehabilitation exercises (such as Kegels and stretches for pelvic floor muscles). Sometimes, a system called “UPOINT” may be used which classifies symptoms into six categories and treats those that are specifically present (Urinary, Psychological/Social, Organ specific, Infection, Neurological and Tenderness).
Risk Factors: Some potential factors include age, having previously suffered from prostatitis, conditions that predispose individuals to UTIs (urinary tract infections), having HIV or AIDS, use of catheters or invasive medical procedures, and prostate biopsies.
Frequency: Chronic pain syndrome affects 1 in 3 men who have been assigned a male at birth (AMAB) and is one of the most frequent urinary tract issues in men. It can be experienced at any point in adult life, with older adults (over 50) more prone due to enlarged prostate.
Complications: Prostatitis can lead to more serious problems if left untreated. Complications of bacterial prostatitis include spread of the infection to other body parts, such as blood (sepsis), reproductive organs, or the bladder, and the development of a pus-filled prostate cavity (prostatic abscess). Chronic forms of prostatitis may cause depression, sexual dysfunction, and infertility. However, there is no proven connection between prostatitis and prostate cancer.
Management and Prevention: Seek prompt medical attention if you experience urinary or genital discomfort, as this can signify prostatitis. Treatment involves addressing any underlying bacterial infection with appropriate antibiotics, managing symptoms through lifestyle changes, and providing education to reduce stress. It’s essential to practice good genital hygiene and engage in safe sexual practices to lower the risk of prostatitis and UTIs.
What are two causes of prostatitis?
Two primary causes of prostatitis include bacterial infections and nonbacterial inflammation.
Acute bacterial prostatitis, a severe form, is often caused by common strains of bacteria such as Escherichia coli. These bacteria can spread from other parts of the urinary or reproductive systems to the prostate.
Nonbacterial prostatitis may result from stress, nerve inflammation or irritation, injuries, or previous urinary tract infections. The condition lacks bacterial presence in urine or seminal fluid.
Acute bacterial prostatitis requires immediate medical attention as it may cause complications like sepsis. In contrast, chronic nonbacterial prostatitis can be difficult to treat, and the main goal is to control symptoms rather than cure the condition.
What are the symptoms of prostate infection?
The most common signs and symptoms of prostatitis can include:
- Chronic bacterial prostatitis symptoms:
- Frequent urination (up to 8 times a day).
- Pain during urination.
- Pain in the genital area, groin, lower abdomen, or lower back.
- Painful ejaculation.
- Urinary retention (inability to empty the bladder completely).
- Trouble starting a urine stream.
- Urinary blockage (complete inability to urinate).
- Chronic prostatitis/chronic pelvic pain syndrome symptoms:
- Pain in the pelvic area.
- Pain between the scrotum and anus.
- Central lower abdomen pain.
- Pain in the penis.
- Pain in the scrotum.
- Pain in the lower back.
- Pain during or after ejaculation.
- Pain in the urethra during or after urination.
- Urinary frequency (8 or more times a day).
- Urinary urgency (inability to delay urination).
- A weak or interrupted urine stream.
- Acute bacterial prostatitis symptoms:
- Severe symptoms that require immediate medical care.
- Frequent urination.
- Urinary urgency.
- Fever.
- Chills.
- A burning feeling or pain during urination.
- Pain in the genital area, groin, lower abdomen, or lower back.
- Nocturia (frequent urination during sleep).
- Nausea and vomiting.
- Body aches.
- Urinary retention.
- Trouble starting a urine stream.
- A UTI (urinary tract infection) as shown by bacteria and infection-fighting cells in the urine.
How can I avoid getting prostatitis again?
To avoid getting prostatitis again, it is essential to take a proactive approach in maintaining prostate health. Here are some measures to lower the risk of recurrence:
- Maintain good hygiene: Keep the genital area clean by washing daily with warm water and a mild, unscented soap. Always wipe from front to back to avoid transferring bacteria from the anus to the urethra.
- Regularly empty the bladder: It is crucial to urinate as soon as the urge arises to prevent bacteria from building up in the urinary tract.
- Hydrate adequately: Staying well-hydrated helps ensure that urine flows freely and bacteria are flushed out regularly.
- Practice safe sex: Using condoms during sexual activity can help prevent sexually transmitted infections (STIs) that may lead to prostatitis.
- Manage stress and engage in regular exercise: Stress has been linked to an increased risk of prostatitis. Regular exercise can help reduce stress levels and improve overall well-being.
- Take antibiotics as prescribed: If you have been diagnosed with bacterial prostatitis, it is vital to complete the full course of antibiotics, even if symptoms improve before the prescribed treatment period ends. This will help ensure that the infection is fully eradicated and reduce the risk of recurrence.
- Consider lifestyle modifications: Some studies suggest that a diet rich in fruits, vegetables, and low-fat dairy products may help reduce the risk of prostatitis. Limiting spicy foods, alcohol, and caffeine may also be beneficial.
It is essential to consult a healthcare provider for guidance on managing prostatitis and preventing recurrence. Regular check-ups can help identify any potential issues early and ensure proper treatment.
How do you flush out a prostate infection?
To effectively address a prostate infection (Prostatitis), follow these recommendations:
- Seek medical care: Consult a healthcare provider to diagnose and recommend appropriate treatment options for the prostate infection. The diagnosis will typically involve physical exams, urine tests, blood tests, and possibly a prostatic specimen test.
- Antibiotics: If the prostate infection is bacterial in nature, antibiotics will likely be prescribed, sometimes for 6-8 weeks, depending on the severity and the type of bacteria responsible for the infection.
- Prostate massage: In certain instances, a healthcare provider may gently massage the prostate during a rectal examination to release prostate fluid into the urethra. The fluid is then expelled through urine for further bacterial testing.
- Stay hydrated: Drinking plenty of water is recommended, as it increases urine output, aiding in the flushing of bacteria from the urinary system.
- Lifestyle modifications: Some changes in your daily routine can help alleviate prostatitis symptoms, such as limiting alcohol, caffeine, spicy or acidic foods, and maintaining a balanced diet.
- Heat therapy: Soaking in a warm bath or using a heating pad might provide relief from the discomfort and inflammation caused by prostatitis.
- Ongoing support: If treatment is prolonged, it may be necessary to have regular follow-up visits with your healthcare provider to ensure the infection has been eliminated and that there are no complications.
Can you live a normal life with prostatitis?
Prostatitis, particularly the chronic abacterial type, is a troublesome condition that can negatively impact a man’s quality of life. Despite being able to live a relatively normal life, it can be difficult, and the people around them are often unaware of the challenges they face.
The symptoms can cause severe pain and frequent mood fluctuations, leading to social isolation, restrictions at work, and difficulties during leisure activities. Accepting the situation and developing coping strategies are essential challenges for individuals suffering from chronic abacterial prostatitis.
Prompt healthcare attention is essential if you’re experiencing pain or changes while urinating, as delaying treatments may make the condition more severe. Consulting medical professionals like Dr. Samarth Agarwal can prevent complications in prostatitis, and make sure it does not impact an individual’s quality of life.